A bone density test is a medical exam that measures the density of bones to determine if they are healthy or at risk of fractures. Bone density tests are typically performed to diagnose osteoporosis, a condition in which bones become weak and brittle and are at an increased risk of fractures.
This article will explore everything you need to know about a bone density test procedure. We urge you to get the best gynecological care in Margate, Florida, if you have any concerns about your health and well-being.
How Is Osteoporosis Diagnosed?
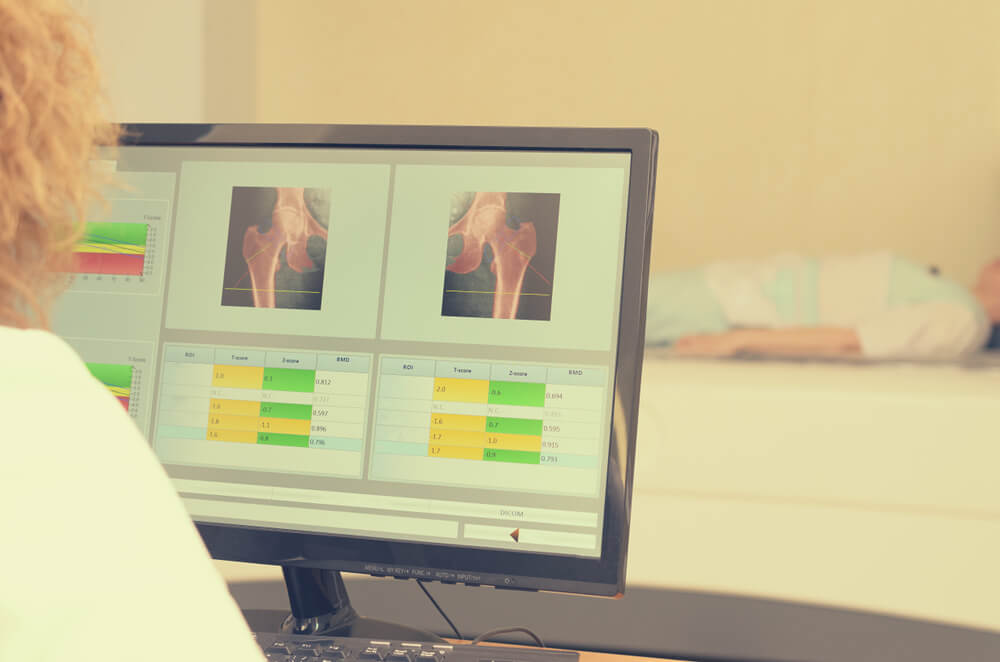
Osteoporosis is diagnosed through a bone density test, which is a non-invasive procedure that calculates the amount of minerals, mainly calcium, located in the bones. The test uses a low-dose X-ray, called dual-energy X-ray absorptiometry (DXA), to measure mineral bone density at different sites in the body, such as the hip and spine.
The World Health Organization (WHO) has established a diagnostic criterion for osteoporosis based on DXA measurements. According to the WHO, a T-score of -2.5 or lower indicates osteoporosis. In contrast, that between -1.0 and -2.5 indicates osteopenia, a condition of low bone density that is not severe enough to be classified as osteoporosis.

Can You Reverse Osteoporosis?
So, can osteoporosis be reversed? While there is no cure for osteoporosis, there are treatments that can help slow down or even reverse bone loss.
The most effective way to reverse or prevent further bone loss is through a combination of lifestyle changes and medications. Regular exercise, especially weight-bearing and strength-training exercises, can help improve bone density and reduce the risk of fractures. Adequate calcium and vitamin D intake are also crucial for bone health. Sometimes, your doctor may recommend medications such as bisphosphonates, teriparatide, or denosumab to help improve bone density and reduce the risk of fractures. However, these medications have potential side effects and should only be taken under the supervision of a healthcare professional.
While it may not be possible to reverse osteoporosis, early diagnosis and treatment completely can help prevent further bone loss and reduce the risk of fractures.
How the Test Works
A bone density test is a quick, painless, and non-invasive procedure that measures the density of your bones using low-dose X-rays. The test is typically performed on the hip, spine, and sometimes the forearm. During the bone density scan, you will lie on a padded table while a machine scans the target area. This takes only a few minutes to complete, and the bone density test results are available immediately.
The DXA machine measures bone density by emitting two low-dose X-ray beams, which the bone and soft tissue absorb differently. The difference in absorption allows the machine to calculate the amount of mineral in the bone. The amount of mineral is then compared to the average mineral content for someone of your age, gender, and ethnicity to determine your T-score.
Who Needs to Get Tested
The National Osteoporosis Foundation (NOF) recommends that all women older than 65 and men older than 70 should get a bone density scan. If you are younger than 65 and have osteoporosis risk factors, such as low body weight, a history of fractures and/or osteoporosis in the family, or early menopause, you may also need to go through a bone density test procedure.
In addition, if you have been on long-term steroid therapy or have a condition that affects bone health, such as hyperparathyroidism or kidney disease, you, too, may need a bone density scan. Your doctor will determine if you need this test based on your individual risk factors.
Can DXA Do More Than Measure Bone Density?
DXA can also measure body composition, including the percentage of body fat and lean muscle mass. This information can help assess overall health and fitness, especially in athletes or people with obesity.
Are There Other Tests for Bone Density and Bone Health?
In addition to DXA, there are other tests that can assess bone health, including quantitative computed tomography (QCT) and peripheral dual-energy X-ray absorptiometry (pDXA). QCT is a more advanced form of DXA that measures bone density in three dimensions and can provide information on bone strength and geometry. pDXA is a portable version of DXA that is used for measuring bone density in the wrist, heel, or finger.
There are also blood tests that can assess bone health, such as the serum bone turnover markers test, which measures the levels of specific proteins in the blood that are related to bone metabolism. However, these are not used for diagnosing osteoporosis but typically to monitor the response to osteoporosis treatment.
Bone Density Test Preparation Process
Before your bone density test, you should wear comfortable clothing without metal, such as zippers, snaps, or buttons, as they can interfere with the test. You should also avoid taking calcium supplements, multivitamins, or antacids containing calcium for at least 24 hours before the test, as they can affect the results.
If you have had a recent X-ray or CT scan that involved contrast material, part of your bone density test preparation involves waiting at least two weeks before getting it done, as the contrast material can interfere with the test results.

The Meaning of Your Bone Density Test Results
Your bone density test results will be shown as a T-score. This score matches your bone density against that of a young and healthy adult of the same gender. A T-score of -1.0 or higher is thought to be normal. If this number falls somewhere between -1.0 and -2.5, you have osteopenia, which means that your bone mass is on the lower end. In the case of a -2.5 or even lower score, it all points to osteoporosis.
Your doctor will use your T-score and other factors, such as your age, sex, and family history, to determine your risk of fractures and recommend the appropriate treatment. Treatment for osteoporosis may include lifestyle changes, such as exercise and diet modifications, as well as medications to improve bone density and reduce the risk of fractures.
How Often Should You Get Tested?
The frequency of bone density testing depends on your individual risk factors for osteoporosis. If you have normal bone density or osteopenia and no significant risk factors, the NOF recommends getting a bone density test every five to ten years. If you have osteoporosis or a high fracture risk, your doctor may recommend more frequent testing.
The Bottom Line
A bone density test is a non-invasive, painless procedure that measures the density of bones to assess their health and risk of fractures. It is typically performed to diagnose osteoporosis, a condition in which bones become weak and brittle and are at an increased risk of fractures. Your doctor will use your bone density test results and other factors to determine your risk of fractures and recommend the appropriate treatment.
In case you fear you’re at risk of osteoporosis or have any other health concerns, don’t hesitate to contact us at Fern F. Taisenchoy-Bent, MD LLC, and schedule your appointment.