Surgeon in Tampa Bay
What is a Hysterectomy
Hysterectomy is a surgery to remove a woman’s uterus (her womb). The whole uterus with cervix is usually removed. Your doctor also may remove your fallopian tubes and ovaries.
Talk to your doctor before your surgery to discuss your options. For example, if both ovaries are removed, you will have symptoms of menopause. Ask your doctor about the risks and benefits of removing your ovaries.
Why would I need a Hysterectomy?
You may need a hysterectomy if you have one of the following:1
- Uterine fibroids. Uterine fibroids are noncancerous growths in the wall of the uterus. In some women they cause pain or heavy bleeding.
- Heavy or unusual vaginal bleeding. Changes in hormone levels, infection, cancer, or fibroids can cause heavy, prolonged bleeding.
- Uterine prolapse. This is when the uterus slips from its usual place down into the vagina. This is more common in women who had several vaginal births, but it can also happen after menopause or because of obesity. Prolapse can lead to urinary and bowel problems and pelvic pressure.
- Endometriosis. Endometriosis happens when the tissue that normally lines the uterus grows outside of the uterus on the ovaries where it doesn’t belong. This can cause severe pain and bleeding between periods.
- Adenomyosis. In this condition the tissue that lines the uterus grows inside the walls of the uterus where it doesn’t belong. The uterine walls thicken and cause severe pain and heavy bleeding.
- Cancer (or precancer) of the uterus, ovary, cervix, or endometrium (the lining of the uterus). Hysterectomy may be the best option if you have cancer in one of these areas. Other treatment options may include chemotherapy and radiation. Your doctor will talk with you about the type of cancer you have and how advanced it is.
What are the different types of Hysterectomies?
- A total hysterectomy removes all of the uterus, including the cervix. The ovaries and the fallopian tubes may or may not be removed. This is the most common type of hysterectomy.
- A partial, also called subtotal or supracervical, hysterectomy removes just the upper part of the uterus. The cervix is left in place. The ovaries may or may not be removed.
- A radical hysterectomy removes all of the uterus, cervix, the tissue on both sides of the cervix, and the upper part of the vagina. A radical hysterectomy is most often used to treat certain types of cancer, such as cervical cancer. The fallopian tubes and the ovaries may or may not be removed.
How is a Hysterectomy Performed?
A hysterectomy can be done in several different ways. It will depend on your health history, the reason for your surgery and your surgeon’s skill level. Talk to your doctor about the different options:
- Abdominal hysterectomy. Your doctor makes a cut, usually in your lower abdomen.
- Vaginal hysterectomy. This is done through a small cut in the vagina.
- Laparoscopic hysterectomy. A laparoscope is an instrument with a thin, lighted tube and a small camera that allows your doctor to see your pelvic organs. Laparoscopic surgery is when the doctor makes very small cuts to put the laparoscope and surgical tools inside of you. During a laparoscopic hysterectomy the uterus is removed through the small cuts made in either your abdomen or your vagina.
Robotic surgery. Your doctor guides a robotic arm to do the surgery through small cuts in your lower abdomen, like a laparoscopic hysterectomy.
Surgical Intervention
Surgical care can be broadly classified as conservative when reproductive potential is retained, semiconservative when reproductive ability is eliminated but ovarian function is retained, and radical when the uterus and ovaries are removed. Age, desire for future childbearing, and deterioration of quality of life are the main considerations when deciding on the extent of surgery.
Surgical efforts are aimed at removal of the endometrial implants and correction of anatomic distortions. Implants can be ablated using either laser energy or electrosurgical techniques.
Resection of the implants and adjacent peritoneum is considered the treatment of choice by some authors. A radical surgical approach involves total hysterectomy and bilateral salpingo-oophorectomy (TAH-BSO). This is generally reserved for women who have completed their family or for women with severely disabling pain that is unresponsive to more conservative approaches.
Conservative Surgery
With conservative surgery, the aim is to destroy visible endometriotic implants and lyse peritubal and periovarian adhesions that are a source of pain and may interfere with ovum transport. The laparoscopic approach is the method of choice for treating endometriosis conservatively.
Ablation can be performed with laser or electrodiathermy. Overall, the recurrence rate is 19% and is similar for all techniques. Laparoscopic ablative surgery with bipolar diathermy or laser for endometriomas was shown to be effective for relieving pelvic pain in 87% of patients.
Postoperative adjunctive hormone therapy
For patients with mild disease, postoperative adjunctive hormonal treatment has been shown effective in reducing pain but has no impact on fertility. GnRH analogues, danazol, and medroxyprogesterone have all been found to be useful for this indication. However, for severe endometriosis, the efficacy of preoperative or postoperative hormonal treatment has not yet been established.
Semiconservative Surgery
The indication for this semiconservative surgery is mainly in women who have completed their childbearing, are too young to undergo surgical menopause, and are debilitated by the symptoms. Such surgery involves hysterectomy and reduction of pelvic endometriosis.
Ovarian endometriosis can be removed surgically, because one tenth of functioning ovarian tissue is all that is needed for hormone production.
Medical therapy in women who have completed childbearing is equally efficacious for symptom suppression.
Radical Surgery
Radical surgery involves total hysterectomy with bilateral oophorectomy and reduction of visible endometriosis. Adhesiolysis is performed to restore mobility and normal intrapelvic organ relationships.
Overview
The normal ovary by nature is a partially cystic structure. Most ovarian cysts develop as consequence of disordered ovulation in which the follicle fails to release the oocyte. The follicular cells continue to secrete fluid and expand the follicle, which over time can become cystic.
The ovaries are the female pelvic reproductive organs that house the ova and are also responsible for the production of sex hormones. They have paired organs located on either side of the uterus within the broad ligament below the uterine (fallopian) tubes. The ovaries are responsible for housing and releasing ova, or eggs, necessary for reproduction.
Most cysts spontaneously resolve while some will persist. The persistent ovarian cysts are most likely to be surgically managed. The standard surgical approach to presumptively benign ovarian cysts is the laparoscopic/Robotic ovarian cystectomy. It is one of the most common procedures performed by the practicing obstetrician-gynecologist.
Surgical Treatments
If your symptoms are severe and nonsurgical treatments haven’t helped, you may want to consider surgery. There are two types of prolapse surgery: obliterative and reconstructive.
Obliterative surgery narrows or closes off part or all of the vagina. The goal is to provide more support to the organs that have dropped out of their normal positions and are pressing against the walls of the vagina. This may be an option if surgery hasn’t worked and you can’t tolerate another procedure, or if you are not healthy enough to have bigger surgery to correct the problem. After this operation you will no longer be able to have intercourse.
Reconstructive surgery aims to repair the pelvic floor and return organs to their original position. This can be done with cuts either in the vagina or the abdomen. It can also be done using laparoscopic surgery, in which a surgeon makes smaller cuts in the abdomen and uses special instruments.
There are a number of reconstructive surgeries your doctor can perform to restore the appearance and function of your pelvic organs. Please schedule a consultation to see if surgery is the right option for you.
Urinary incontinence surgery in women: The next step
If you have severe symptoms of stress urinary incontinence or overactive bladder, surgery may provide a permanent solution to your problems. But surgery isn’t for everyone. Find out what procedures may help in treating urinary incontinence.
For some women, symptoms of stress incontinence or overactive bladder don’t respond to conservative treatment. When you’ve tried conservative measures and urinary incontinence continues to disrupt your life, surgery might be an option.
Urinary incontinence surgery is more invasive and has a higher risk of complications than do many other therapies, but it can also provide a long-term solution in severe cases.
The surgical options available to you depend on the type of urinary incontinence you have. Most options for urinary incontinence surgery treat stress incontinence. However, low-risk surgical alternatives are available for other bladder problems, including overactive bladder — also called urge incontinence or urgency-frequency syndrome.
Things to consider
Before you choose urinary incontinence surgery:
- Get an accurate diagnosis. Different types of incontinence require different surgical approaches. Your doctor might refer you to an incontinence specialist, urologist or urogynecologist for further diagnostic testing.
- Think about your plans for having children. Your doctor might recommend waiting for surgery until you’re finished with childbearing. The strain of pregnancy and delivery on your bladder, urethra and supportive tissues might undo the benefits of a surgical fix.
- Understand that surgery only corrects the problem it’s designed to treat. Surgery doesn’t cure all urinary incontinence. For instance, if you have mixed incontinence — a combination of stress incontinence and overactive bladder — surgery might improve your stress incontinence but not your overactive bladder. You might still need medication and physical therapy after surgery to treat overactive bladder.
Understand the risks
Like any surgery, urinary incontinence surgery comes with risks. Although uncommon, potential complications include:
- Temporary difficulty urinating and incomplete bladder emptying (urinary retention)
- Development of overactive bladder, which could include urge incontinence
- Urinary tract infection
- Difficult or painful intercourse
One step at a time
Finding an effective remedy for urinary incontinence might take time, with several steps along the way. If conservative treatment isn’t working for you, ask your doctor if there might be another solution to your problem.
Schedule a consultation and ask your doctor about the possible risks and benefits of surgery.
Laparoscopic Sterilization Procedure
Surgical approaches for female sterilization include laparoscopy, hysteroscopy, microlaparoscopy, laparotomy (concurrent with cesarean delivery), mini-laparotomy. Although mini-laparotomy is the most common approach worldwide, laparoscopy is used most commonly for interval procedures in the United States.
In laparoscopy, an instrument called a laparoscope is inserted through a small incision made in or near the navel. Another small incision may be made for an instrument to close off or remove the fallopian tubes. The fallopian tubes can be closed off by bands or clips. They also can be cut and closed with a special thread or sealed with an electric current. The laparoscope then is withdrawn. The incisions are closed with stitches.
Laparoscopy has some benefits over mini-laparotomy. Recovery usually is quicker. There are fewer complications. It usually is performed as outpatient surgery, meaning that you can go home the same day.
Why Robotic Surgery?
- Patients may experience fewer complications compared to patients who had open and laparoscopic surgery.
- Patients may stay in the hospital for a shorter amount of time than patients who had open, laparoscopic and vaginal surgery (most go home the same day).
- Surgeons may be less likely to switch to an open procedure when performing surgery with the robot, compared to when performing laparoscopic surgery.
- With robotic surgery, you may have a single or few small incisions compared to an open procedure and, after surgery, one or a few small scars.
What is the “robot” in robotic hysterectomy?
During a robotic hysterectomy, the surgeon uses a state-of-the-art robotic surgical system, but this doesn’t mean the robotic system does the surgery.
This system has multiple “wristed” robotic arms that hold surgical instruments. These arms allow the surgeon to make precise, delicate movements in small spaces. Because the “wrists” on the robotic arms rotate a full 360 degrees, they offer more dexterity than the human hand.
One of the robotic arms holds a tiny 3D, high-definition video camera. This camera broadcasts up-close video of the surgical area to a screen on the system’s control console.
During the procedure, the surgeon maintains complete control of the robot at all times. He or she sits at the control console and maneuvers the robotic surgical instruments, using the real-time video as a guide.
How is a robotic hysterectomy performed?
To begin, the surgeon makes a small incision on the inside rim of the belly button. An additional 2 or 3 small incisions are made in the abdomen to accommodate additional surgical instruments.
After making the incisions, the surgeon uses the robotic arms to insert the video camera and surgical tools. Using the 3D video for guidance, the surgeon maneuvers the surgical instruments with the robotic arms to detach the organs from the surrounding tissues.
After the surgeon detaches the uterus, it’s removed from the body through the vagina or by minimally extending one of the other incisions.
How long is the recovery period?
Most robotic hysterectomy patients return home the same day as surgery with Dr. Stine. Patients regain some mobility the same day of surgery. Ninety percent of patients return to light physical activity and driving within a week and return to desk jobs after 2 weeks.
Even though patients may feel better quickly, it’s important to remember that full recovery takes 6 weeks. To allow the internal sutures to heal during the 6-week recovery, patients shouldn’t insert anything into the vagina or have sex. Patients also should avoid heavy lifting for 4-6 weeks.
How is a robotic hysterectomy different from a laparoscopic or traditional procedure?
A traditional open hysterectomy requires a 5- to 7-inch incision in the abdomen and a 2- to 3-day hospital stay. In addition to a longer recovery time, patients who undergo a traditional open hysterectomy have visible scarring, increased pain and a higher risk of complications, such as infection at the incision site.
A laparoscopic (minimally invasive) hysterectomy is performed through 3 or 4 small incisions in the abdomen. This procedure is less invasive than a traditional open hysterectomy and gives the surgeon a 2D view of the surgical area. Laparoscopic surgical instruments are different in that they don’t give the same full range of motion as the “wristed” robotic arms.
To see if robotic hysterectomy might be right for you, schedule an consultation today
Endometriosis occurs when tissue that lines the uterus migrates outside the uterus, usually to the area around your reproductive organs, including the ovaries or fallopian tubes. Many women with endometriosis have no symptoms. Although for some women, endometrial tissue patches may swell and bleed with their menstrual cycles, which can cause pain. Endometriosis symptoms may include chronic pelvic pain, heavy menstrual bleeding, pain during sex, pain with bowel movements or urination, and fertility issues.
To diagnose endometriosis, doctors may perform a pelvic exam. However, the only way your doctor can provide a definite endometriosis diagnosis is by performing surgery to locate endometrial patches outside the uterus. Rather than put you through multiple surgeries, your surgeon may remove any endometriosis patches he or she finds while performing diagnostic endometriosis surgery.
If you and your doctor decide surgery is right for you, your surgeon will find and remove endometrial patches on and around your ovaries, fallopian tubes, bladder, intestines, and abdomen.
Surgeons can perform endometriosis surgery using traditional open surgery, which requires a long incision (cut) through your abdominal muscles, or through minimally invasive surgery.
There are two minimally invasive approaches: laparoscopic surgery and robotic-assisted surgery. Both are performed through a few small incisions in the abdomen. To perform a laparoscopic endometriosis procedure, surgeons use special long-handled tools while viewing magnified images from the laparoscope (camera) on a video screen.
Surgeons can perform robotic-assisted endometriosis surgeries using a robotic system. During endometriosis surgery with the robot, your surgeon sits at a console next to you and operates using tiny, fully wristed instruments.
A camera provides a high-definition, 3D magnified view inside your body. Every hand movement your surgeon makes is translated by the robotic system in real time to bend and rotate the instruments with precision.
To see if you are a candidate for Robotic Endometriosis resection, schedule a consultation today
Fibroids
- Intramural fibroids: These are the most common type of fibroids. Intramural fibroids appear in muscular wall of the uterus. Intramural fibroids may grow larger and can stretch your womb. (5)
- Subserosal fibroids: form on the outside of your uterus, which is called the serosa. They may grow large enough to make your womb appear bigger on one side. (5)
- Pedunculated Fibroids: Subserosal tumors can develop a stem, a slender base that supports the tumor. When they do, they’re known as pedunculated fibroids. (5)
- Submucosal Fibroids: These types of tumors develop in the middle muscle layer, or myometrium, of your uterus. Submucosal tumors aren’t as common as the other types. (5)
Fibroid symptoms are often caused by the consistency, size, and location of the fibroid.
Women experience a variety of symptoms from fibroids that can become extremely debilitating and affect their everyday lives. Symptoms such as heavy and painful periods, periods lasting longer than 7+ days, stomach, lower-back, and pelvis pain, stomach protrusion which causes women to look pregnant when they aren’t, anemia, infertility, painful sex, urinary frequency, and G.I. issues like gas and constipation.
Between 15-30% of women experience severe pain and discomfort daily from their fibroids. (6)
Women are typically between the ages of 35-55 when they develop fibroids. (7) Though this is the most common age, women can develop fibroids at any stage of their life.
What Are Uterine Fibroids?
Uterine fibroids, which your doctor may call leiomyomas or myomas, are muscular tumors that can grow on your uterus. They rarely turn into cancer, and if you get them it doesn’t mean you’re more likely to get uterine cancer.
Fibroids can vary a lot in size, shape, and location. They can show up in your uterus, uterine wall, or on its surface. They can also attach to your uterus by a stalk- or stem-like structure.
Some are so small that your doctor can’t even see them with the naked eye. Others grow in big masses that can affect the size and shape of your uterus.
Uterine fibroids usually appear in women of childbearing age — generally between 30-40 years old, but they can show up at any age. They’re more common in African American women than in white women, and they also tend to show up earlier and grow quicker in African American women.
What is a Myomectomy?
Myomectomy is a surgery to remove fibroids. If you plan to become pregnant, your doctor may recommend this over other procedures. But it may cause scarring that can lead to infertility. You’ll need to wait 4 to 6 months after surgery before you try to conceive. In most women, symptoms go away following a myomectomy. But in others, the fibroids come back. Whether it works will partly depend on how many fibroids you have and whether the surgeon could remove them all. A myomectomy may be abdominal surgery, or your surgeon may use a hysteroscope or laparoscope/Robotic surgery to remove the fibroids without having to make a large cut on your abdomen.
WHAT’S THE GOAL OF THE PROCEDURE?
A uterus can have fibroids and still be healthy. The truth is 70% of women have fibroids. When fibroids cause disruptive symptoms, women have options.
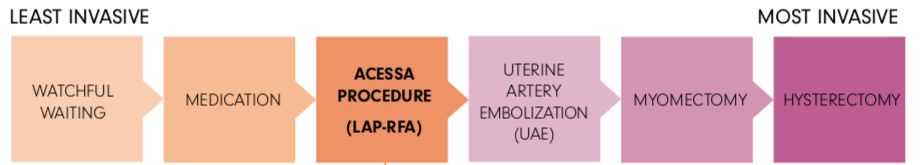
That’s where we come in. The Acessa procedure was designed to maintain the integrity of the uterus by focusing treatment solely on the fibroid (vs. cutting into the uterus or removing it completely) and more importantly to relieve symptoms caused by fibroids.
This is done by applying controlled heat directly into the fibroid, which in turn destroys the fibroid tissue and causes it to shrink over time (imagine the consistency of a baseball changing to a marshmallow). The smaller and softer destroyed fibroid tissue leads to symptom relief, without having to cut open your uterus.
A robotic-assisted myomectomy is a type of surgery. It is done to remove growths in a woman’s uterus called fibroids. The surgery is done with special tools.
The uterus is a reproductive organ in a woman’s lower belly (abdomen). A baby grows inside the uterus during pregnancy. Sometimes, cells from the inside walls of the uterus grow and form tumors called fibroids (also called leiomyomas or myomas). Fibroids are almost always not cancer (benign). They can be very small, or as large as a grapefruit. Fibroids are very common. Your risk of fibroids increases with age until you reach menopause.
Fibroids can grow on the outer part of the uterus, within the wall of the uterus, or stick out into the inside of the uterus. One or more fibroids can grow at the same time in different places in the uterus. Fibroids are usually not cancer. But they can still cause problems. Surgery is then done to remove them.
Robotic-assisted myomectomy is one type of surgery to remove fibroids. It is a minimally invasive method. This means it uses smaller incisions than a standard surgery. It’s done while you’re asleep under general anesthesia.
During the surgery, your doctor will put small tools and a tiny camera through small incisions on your lower belly. This gives your doctor a better view of the area in your body. Your doctor moves the tools using a robotic controller. This lets your provider make very small movements with the tools. The doctor removes the fibroids from your uterus. The tools are then removed. The incisions are closed and bandaged.
Robotic-assisted myomectomy has some benefits over other methods. It may have a lower risk of complications for some people. It can lead to a shorter hospital stay and a faster recovery time. The surgery may also allow a provider to remove fibroids that are hard to remove with another method.
To see if you are a candidate for a robotic myomectomy, schedule a consultation today
Acessa Procedure for Fibroids
Who is this procedure for?
This procedure is for pre-menopausal women (typically younger than 55 years old) who are tired of living with the ongoing pain and discomfort of fibroids and are looking for a minimally invasive option that allows them to keep their uterus and return to daily life quickly after the procedure.
Patient Feedback
Marina D.
Dr. Stine is the best Gyn I’ve ever had in all my 53 years! He’s caring and compassionate and listens to me and has the highest professionalism and ethics. His skills in the OR are superb from my personal experience providing me with a newly found quality of life! I have recommended him to my family and will also be taking my daughters to him. That’s how much trust I have in him!
Valerie S.
Dr. Stine is the absolute best! He is thorough, so comforting and knows his stuff! He truly cares about his patients and takes such great care of us. He is a blessing to all his patients.
Melissa D.
My experience with Dr. Stine was basically perfect! I know a lot of women, myself included, that are not comfortable with a male doctor. Dr. Stine changed that for me!
I felt so at ease with him, his bedside manner is amazing. His surgical skills are TOP NOTCH! Do yourself a favor and become a patient of his!
Request an Appointment
Have a question about our practice or want to schedule an appointment? Reach out and speak with a member of our team.